By BCN Executive Editor Wesley Brown – May 29, 2022 – There’s good news and a lot of not-so-good news on the cancer front when it comes to Black patients in recent research and progress.
On the good news side, new data released May 19 by the National Cancer Institute (NCI) shows that from 1999 to 2019 that cancer death rates declined steadily among Black people in the U.S. Nevertheless, in 2019, Black people still had considerably higher rates of cancer death than people in other racial and ethnic groups, a large epidemiologic study has found.
The study was led by researchers at the National Cancer Institute, part of the National Institutes of Health, and the findings appeared on May 19 in JAMA Oncology.
“Even though there has been a decline in cancer mortality nationally among Black people, they continued to bear a higher cancer burden overall than all other racial and ethnic groups studied,” said Dr. Wayne Lawrence of the Metabolic Epidemiology Branch in NCI’s Division of Cancer Epidemiology and Genetics, who led the study.
Lawrence and his colleagues used death certificate data from the National Center for Health Statistics to analyze age-adjusted cancer death rates by age, sex, and cancer site among non-Hispanic Black people ages 20 and older in the United States. They then compared cancer death rates in 2019 among Black men and women with those in other racial and ethnic groups.
Between 1999 and 2019, more than 1 million Black men and women ages 20 and older died of cancer. During that period, cancer death rates among this group decreased by 2% per year, with a more rapid decrease among men (2.6% per year) than women (1.5% per year).
Death rates declined for most cancer types; the most rapid decreases were in lung cancer among men (3.8% per year) and stomach cancer among women (3.4% per year). However, over the same 20-year period, deaths from liver cancer increased among older Black men and women and deaths from uterine cancer increased among Black women.
Dr. Lawrence noted that the overall decline in cancer death rates in Black people could be due to some combination of improved access to screening, earlier detection, advances in treatment, and behavioral changes, such as declines in cigarette smoking.
In their comparison of cancer death rates among racial and ethnic groups in 2019, the researchers found that Black men and women had higher rates of cancer death, both overall and for most cancer types, than white, Asian or Pacific Islander, American Indian/Alaska Native, and Hispanic/Latino men and women.
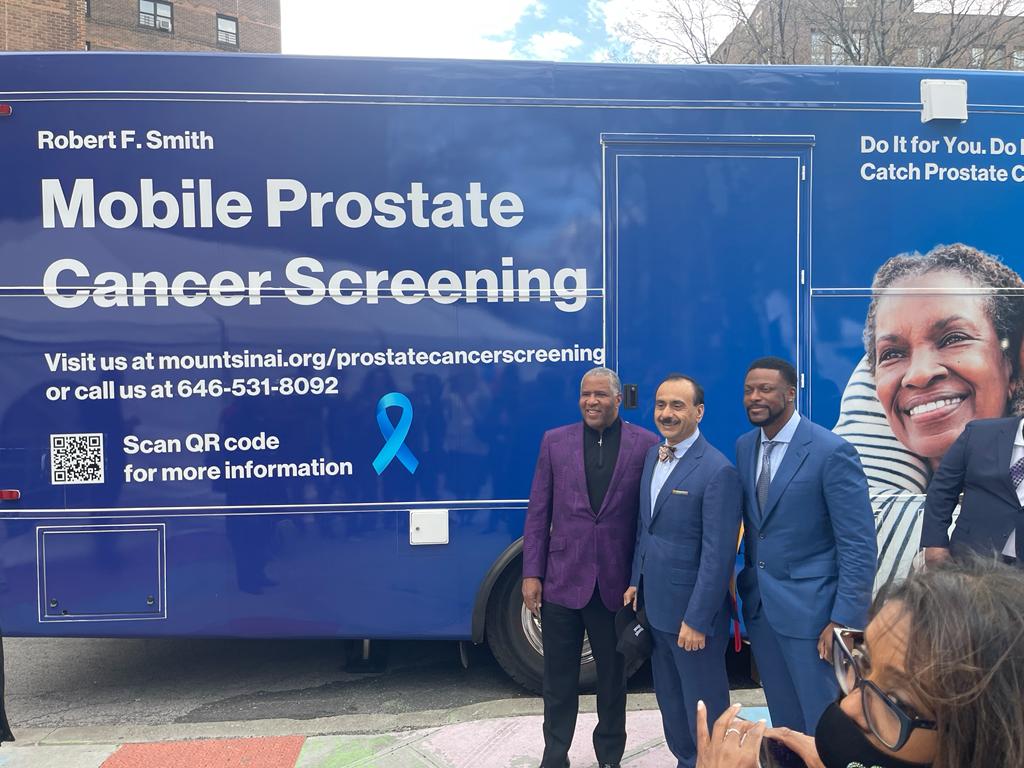
For example, the prostate cancer death rate among Black men was nearly five times higher than among Asian or Pacific Islander men. The breast cancer death rate among Black women was nearly 2.5 times higher than among Asian or Pacific Islander women.
“The disparity in deaths likely reflects systemic and preventable barriers to getting quality care. Whether it’s screening for cancer, timely diagnosis, or the receipt of proven treatments,” Lawrence explained. “Black individuals continue to have a delay in care or receive poorer care than their white counterparts.”
One limitation of the study is the broad groupings used for race and ethnicity, which could make it harder to tease out differences among people who are racially categorized as Black, Lawrence said. Another limitation is the potential misclassification of race and ethnicity and the underlying cause of death recorded on death certificates.
One cause for concern, he noted, is the disproportionate effect of COVID-19 on access to cancer-related medical care in Black communities in the United States, such as a larger decline in breast cancer screening among Black women compared with white women.
“These factors could cause the decline in cancer death rates among Black individuals to slow in coming years,” Lawrence said.
Clinical trial
Meanwhile, a separate study conducted by researchers from VCU Massey Cancer Center in Richmond, Va., the University of Florida College of Medicine and UF Health Cancer Center in Gainesville, Fla., found that minority patient participation in cancer clinical trials is alarmingly low. In the U.S., clinical trials are responsible for determining the safety and efficacy of drugs and lead to virtually all standards of cancer care in the U.S.
This significant disparity creates a substantial gap between the patient populations in which the drugs are tested and those that are treated after drugs are federally approved. One reason for this gap is standard clinical trial criteria that disproportionately exclude Black patients.
In recent findings published in the Journal of Clinical Oncology, the researchers determined that traditional eligibility criteria — a set of standardized requirements that must be met for a patient to enroll in a clinical trial — disproportionately prevents Black patients from participating in pancreatic cancer clinical trials. Looking at pancreatic cancer patients treated between 2010 and 2019, the researchers found that 42% of Black patients were ineligible for clinical trials compared to 33% of white patients.
“The standard of care in cancer treatment is informed by studies conducted with predominantly non-Hispanic white patients,” said study co-corresponding author Dr. Jose Trevino, surgeon-in-chief at Massey Cancer Center and chair of the Division of Surgical Oncology at the VCU School of Medicine. “Revising the standard criteria for clinical trial enrollment could have a profound effect on increasing eligibility of underserved populations, reducing disparities in trial participation and creating results that are more reflective of the patients that we serve.”
The American Cancer Society estimates that more than 62,000 people will be diagnosed with pancreatic cancer in 2022. Historically, Black, Asian or Pacific Islander, American Indian or Alaskan Native and Hispanic patients have been underrepresented in pancreatic cancer clinical trials. There are a number of known factors that contribute to the underrepresentation of minorities in clinical trials, including distrust in the health care system, systemic racism, lack of diversity among medical providers, and barriers to healthcare access, among others. However, a factor that has been largely ignored is eligibility criteria.
Although criteria are intended to reduce risk and help define a similar patient population, they often inadvertently prevent large subsets of patients from receiving investigational therapies. Medical conditions that can often be medically controlled are associated with underserved populations can exclude many patients from being eligible for a trial, including HIV, hepatitis, chronic kidney disease, diabetes, obesity, and malnutrition.
“These criteria are often not medically justifiable. Given the deadliness of pancreatic cancer, newer, FDA-approved treatments are often administered for cancer patients with these medical conditions despite the absence of such patients in clinical trials,” said study lead author Dr. Andrea Riner, a surgical resident at the University of Florida College of Medicine. “We propose that many of these medical conditions be removed from eligibility criteria for pancreatic cancer clinical trials.”
The study’s authors suggest that collaborating with specialists who can co-manage these additional medical conditions during a cancer clinical trial could allow for more patients to be safely enrolled instead of being denied eligibility.
Because many pancreatic tumors directly trigger diabetes, the researchers propose that uncontrolled diabetes should not exclude a patient from enrolling in a pancreatic cancer clinical trial if they agree to be closely monitored by an additional specialist throughout the trial.
“Diabetes can be well controlled in a relatively short period of time for a majority of patients,” said Trevino, who also holds the Walter Lawrence, Jr., Distinguished Professorship in Oncology at Massey Cancer Center. “However, poorly controlled diabetes may reflect the impact of underlying social determinants of health and inadequate access to care, and thus, clinical trial centers may need to facilitate diabetes care with providers in local communities or via telehealth.”
Additionally, health insurance coverage can affect a patient’s ability to enroll in a clinical trial. Black patients tend to be diagnosed with pancreatic cancer at a younger age than white patients and therefore are less likely to be covered by Medicare. Not all testing and treatment within a clinical trial is wholly covered by the trial or payers, leading some patients to have higher out-of-pocket expenses and further perpetuating disparities in clinical trial participation.
The study authors argue that effectively changing the standards by which eligibility criteria are developed and evaluated cannot be accomplished by individual researchers, but rather through a collective effort by a variety of stakeholders influential to the implementation of clinical trials.
“Everyone has a part to play in changing this. Patient advocacy groups and professional societies can demand policy change; trial funders and regulatory agencies should require medical justification for each eligibility criteria prior to funding or approving a study, and industry partners or other stakeholders should be held accountable for their role in the development of a clinical trial that creates undue barriers for patients to participate,” said study co-corresponding author Dr. Thomas George, FACP, associate director for clinical research at UF Health Cancer Center and professor of medicine at the University of Florida College of Medicine.
The scientific and medical community agrees that diverse participation is not only important for providing equal access to investigational drugs, but it is critical to inform a more comprehensive evaluation of how drugs will affect a wider range of patients. People from different racial and ethnic backgrounds have unique genetic compositions. Therefore, one patient’s treatment resistance or response could be unlike another’s based on their individual genes. Increased diversity in clinical trial participation can potentially help reduce disparities in cancer survivorship.
Although this study looked at pancreatic cancer patients, the researchers believe their findings are likely applicable to clinical trials for other cancer types as they reflect common barriers that are not specific to pancreatic cancer.
Additional collaborators on this research include Nitai Mukhopadhyay, Ph.D., and Tamas Gal, Ph.D., research members at VCU Massey Cancer Center; Nevena Skoro, M.P.H., and Selamawit Girma, M.P.H., of Massey’s Cancer Informatics Core; Dr. Devon Freudenberger, and Dr. Vignesh Vudatha, M.D., of the VCU Department of Surgery; and Kelly Herremans, M.D., of the University of Florida College of Medicine.
This research was supported by the VCU Massey Cancer Center Cancer Informatics Core. Researchers were also supported by the National Human Genome Research Institute; NCI; the Joseph and Ann Matella Fund for Pancreatic Cancer Research; and, in part, by funding from Massey’s NIH-NCI Cancer Center support grant.
The university-led study on clinical trials follows the Biden administration openly expressing concerns about the lack of Black and other minorities that participated in COVID-19 clinical trials earlier this year. On April 13, the U.S. Food and Drug Administration issued new draft guidance on April 13 for developing plans to enroll more participants from underrepresented racial and ethnic populations.
The new FDA order expands on the agency’s previous guidances to improve clinical trial diversity. The most recent guidance was handed down in November 2020 when the Biden administration touted more diversity and inclusion in trials for all medical products related to the highlight touted “Cancer Moonshot” program.
That five-year program was started by the NIH to help researchers better understand and treat cancer. The Moonshot Biobank will ask cancer patients across the U.S. to donate biospecimens or blood and small pieces of tissue removed during medical procedures and associated health information.
On another front regarding cancer and Black patients, the Moffitt Cancer Center in Tampa, Fla., noted publicly as the NIH and university-led cancer news was released that the nation’s Black community faces specific cancer disparities in treatment across the U.S.
For many of the most common types of cancers, including breast, lung, prostate, colorectal, and blood cancers such as multiple myeloma, lymphoma and leukemia, the incidence and/or death rates are higher among Black and African American populations than other racial and ethnic groups.
“The reasons behind those disparities can be many. Access, or lack of access, to cutting-edge treatment, later stage diagnoses, and lack of knowledge are key factors causing cancer disparities in the Black and African American community,” stated the NCI-designated cancer center, noting that it is prioritizing the needs of Black community and emphasizing the importance of screening, early detection, and prevention.
“Moffitt aims to maximize the impact of education and access in our community and beyond by promoting healthy habits with the goal of optimizing outcomes. Moffitt aspires to be part of a paradigm shift that ultimately reduces the cancer burden in the U.S., especially in underserved and underrepresented communities,” said the south Florida cancer center. “There is a time to understand and address health disparities to achieve health equity; that time is now.”
To learn more about how you can get involved or to request community outreach services from Moffitt Cancer Center, visit Moffitt.org/COEE.
(This story is courtesy of Black Consumer News of Arkansas.)


 Sign up as a free Arkansas Delta Informer digital subscriber and get breaking news and weekly news roundup in your inbox.
Sign up as a free Arkansas Delta Informer digital subscriber and get breaking news and weekly news roundup in your inbox.